Das Fachgebiet befasst sich mit der Diagnostik und Behandlung von Herzrhythmus-Störungen. Diese können sich durch Minderung der Leistungsfähigkeit, Kurzatmigkeit, Herzrasen und Herzstolpern, Schwindel und Ohnmacht bemerkbar machen oder sogar zum plötzlichen Herzstillstand und Herztod führen.
The spectrum of possible arrhythmias is as diverse as their symptoms. In recent years, diagnostic and therapeutic procedures have developed rapidly. At Kulmbach Hospital, we offer our patients state-of-the-art examination and therapy methods, such as ablations (catheter-guided ablation) of arrhythmias, including pulmonary vein isolation for atrial fibrillation.
Our treatment focus areas

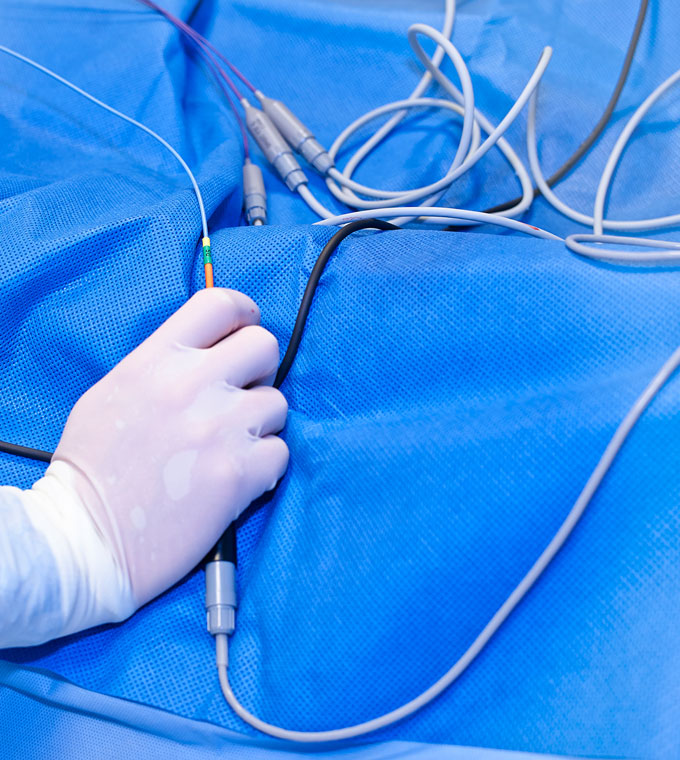
This invasive diagnosis and treatment of arrhythmias is performed using special catheters. Several thin catheters are placed precisely in the heart via the groin vessels under fluoroscopic guidance in order to identify the source and underlying mechanism of an arrhythmia.
Ablation catheters can then be used to selectively destroy areas of the heart muscle in order to prevent the recurrence of tachycardic arrhythmias (i.e. rapid heartbeat). This procedure can permanently cure some arrhythmias, thereby preventing lifelong drug therapy: AV nodal reentry tachycardia (AVNRT), WPW syndrome, atrial tachycardia (AT), atrial flutter, ventricular ectopy.
Pulmonary vein isolation (PVI) can significantly reduce the risk of recurrence of atrial fibrillation, one of the most common arrhythmias. The modern catheter and EPU systems, including a 3D mapping system (CARTO 3), at Kulmbach Hospital enable low-radiation and safe treatment of these conditions.

Pacemakers have been used successfully for many years to treat bradycardic arrhythmias, i.e. conditions characterised by a slow or irregular heartbeat.
These technically advanced devices are now very small, durable, optionally MRI-compatible and equipped with many automatic therapy functions. Implantation is performed under local anaesthetic below the collarbone. From there, one to three thin electrodes (cables) are inserted into the heart via the subclavian vein, as required.

Patients who have suffered severe heart attacks, have severely impaired cardiac output, suffer from ion channel disorders or have been successfully resuscitated are at risk of sudden cardiac death due to ventricular flutter or fibrillation.
Implantable cardioverter defibrillators, or ICDs for short, monitor the heart rhythm and can automatically terminate these life-threatening arrhythmias by means of electrical overstimulation (cardioversion) or shock (defibrillation). Similar to pacemakers, the devices are implanted under or on the chest muscle under local anaesthesia and have at least one electrode connected to the right ventricle.
In suitable cases, we also offer the option of implanting an S-ICD (subcutaneous ICD) into the subcutaneous fatty tissue, which does not require direct electrodes to the heart.
If a patient is only at risk of ventricular fibrillation for a period of weeks or months due to acute heart disease, they can be protected by a portable defibrillation vest (Life Vest).
Many patients with heart failure have a disturbance in the conduction of electrical impulses in the ventricles, also known as left bundle branch block (LBBB).
This electrical conduction disorder causes uneven, rocking contractions (squeezing) of the ventricles. In these cases, the implantation of pacemakers or defibrillators with an additional stimulation electrode in the lateral cardiac vein can restore synchronous (even) contraction and improve cardiac output.
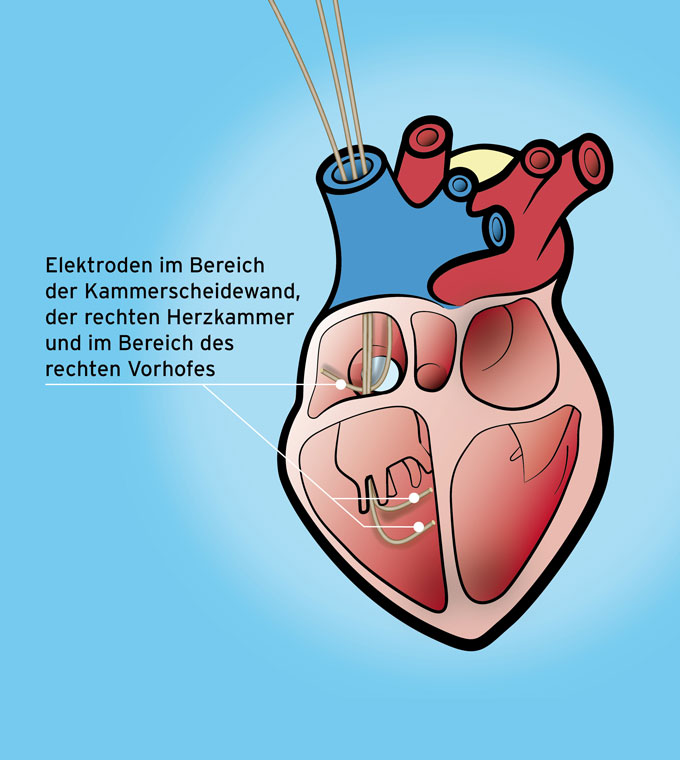
Cardiac contractility modulation is a procedure for treating heart failure when all drug options have been exhausted and other causal therapies have not led to the desired success in cases of significantly reduced cardiac output.
In this form of treatment, two electrodes are implanted in the area of the ventricular septum of the right ventricle and in the area of the right atrium. These are connected to a pacemaker-like device (optimizer), which is usually placed below the right or left collarbone. The implantation technique is almost identical to that used for conventional pacemaker implantation. The device stimulates the heart muscle during the absolute refractory phase. This does not lead to ventricular contraction, but rather to a complex influence on the calcium metabolism of the heart muscle cells. Ultimately, this results in an increase in cardiac output. For patients with severe heart failure, this primarily improves their quality of life and resilience.

Temporary ECG recorder implanted in the size of a matchstick.
This micro device is inserted into the subcutaneous tissue under local anaesthetic and can automatically record arrhythmias over a period of 3 years. The ECG is also transmitted automatically via the mobile phone network to the hospital for evaluation (home monitoring). This procedure is used in particular after unexplained loss of consciousness (syncope) or strokes, which can occasionally be caused by arrhythmias.
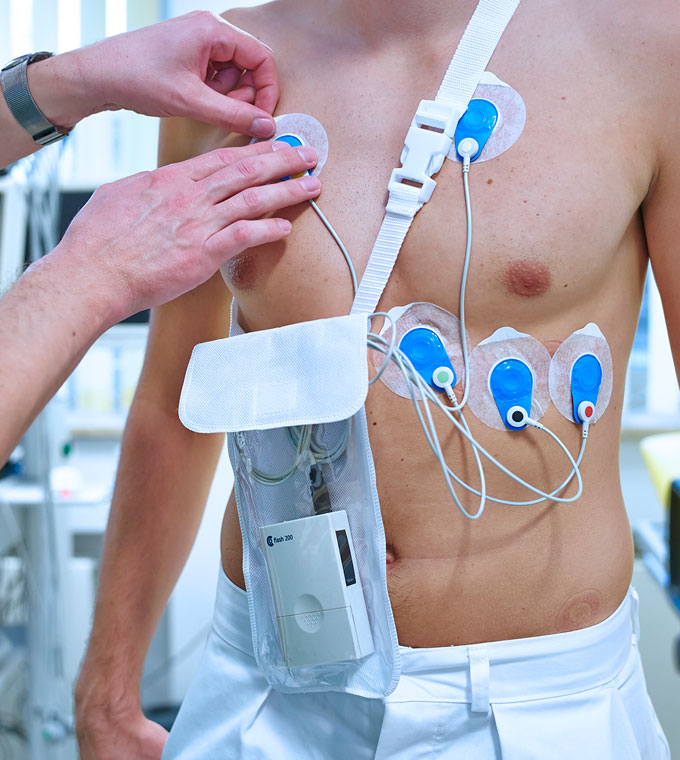
The small recording device, which can be carried in a shoulder bag or on a belt, records ECG signals, either with 3 or 12 leads, over a period of 24 to 72 hours.
The doctor then evaluates the recordings on a computer. The examination is carried out to analyse the rhythm over the course of the day and to record any disturbances that occur in phases.

Continuous ECG radio transmission from the patient to the monitoring and recording monitor in the ward.
The patient carries the transmitter device, which resembles a long-term ECG, in a small shoulder bag. This allows sudden or occasional arrhythmias to be detected immediately.

range of services
- Verödungen bei Herzrhythmusstörungen
- Pulmonalvenenisolation bei Vorhofflimmern
Restoration of normal heart rhythm through electrical impulses or with the help of special medication
Includes home monitoring (Care Link) for recording arrhythmias over a 3-year period
(with electrodes to the heart), also MRI-compatible, for patients with slow or irregular heartbeats
Implantation of defibrillators under the skin without electrodes to the heart (SICD)
Protection against ventricular fibrillation with a portable defibrillation vest
Implantation of pacemakers or defibrillators with an additional stimulation electrode
Implantation of an optimiser (pacemaker-like device) to stimulate the heart muscle when drug and causal therapy for heart failure has been exhausted
- Pacemaker
- Implantable cardioverter defibrillator (ICD)
- Implantable cardiac monitor (ICM)
- Implantable event recorder (ILR)
- Optional home monitoring
certificates




Contact Cardiology and Internal Intensive Care Medicine

Dr. med. Andreas Brugger (englischer Eintrag)
Specialist in internal medicine/cardiology
Additional qualifications:
Interventional cardiology (DGK)
Specialised rhythmology (DGK)
Intensive care
Emergency/rescue medicine
Contact
Albert-Schweitzer-Straße 10
95326 Kulmbach
Cornelia Krauß
Phone 09221 98-1851
Fax 09221 98-1802
E-mail cornelia.krauss@klinikum-kulmbach.de
Office hours and appointments
Please call us to arrange an appointment.


