Non-invasive cardiology refers to treatments and examinations that do not require any intervention in the body. In non-invasive cardiology, we use procedures and medical devices that enable us to assess your heart function and other important bodily functions from the outside.
Non-invasive diagnostic methods such as electrocardiography, ultrasound or long-term blood pressure measurement are an important prerequisite for planning therapeutic measures. Based on the examination results, we can tailor the further treatment process to the needs of our patients.

Elektrokardiographie
By placing a special ultrasound probe on the skin, all structures of the heart are displayed in real time using a black-and-white cross-sectional image.
In particular, the size of the heart chambers, valve function and the pumping function of the heart are clearly visible, allowing the ejection fraction of the heart to be determined. By using various Doppler techniques (colour Doppler, PW and CW Doppler), the function of the heart valves can be assessed, in particular the detection of insufficiencies (leaks) and stenoses (narrowing).

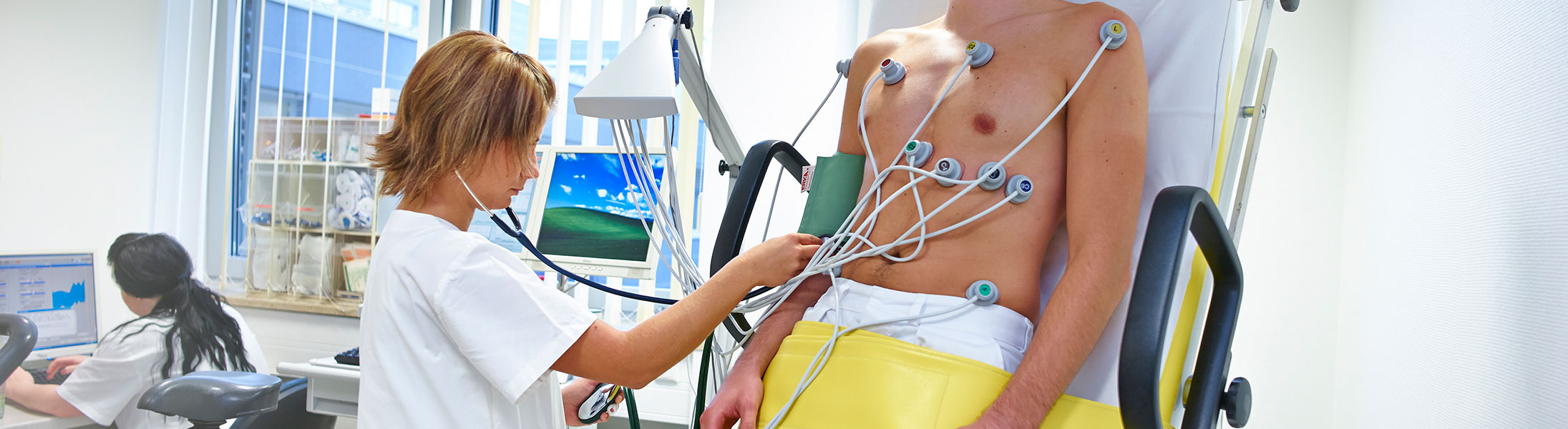
The electrocardiogram is a simple, repeatable and almost universally applicable basic examination in cardiology.
It represents the recording of the sum of the electrical activity of all heart muscle fibres and is used in particular to detect cardiac arrhythmias and circulatory disorders in the heart.

During a stress ECG, the electrocardiogram is recorded during physical activity (on a bicycle or treadmill).
Work performance and possible changes in cardiac and circulatory function are measured, which allows conclusions to be drawn about blood flow to the heart in particular.
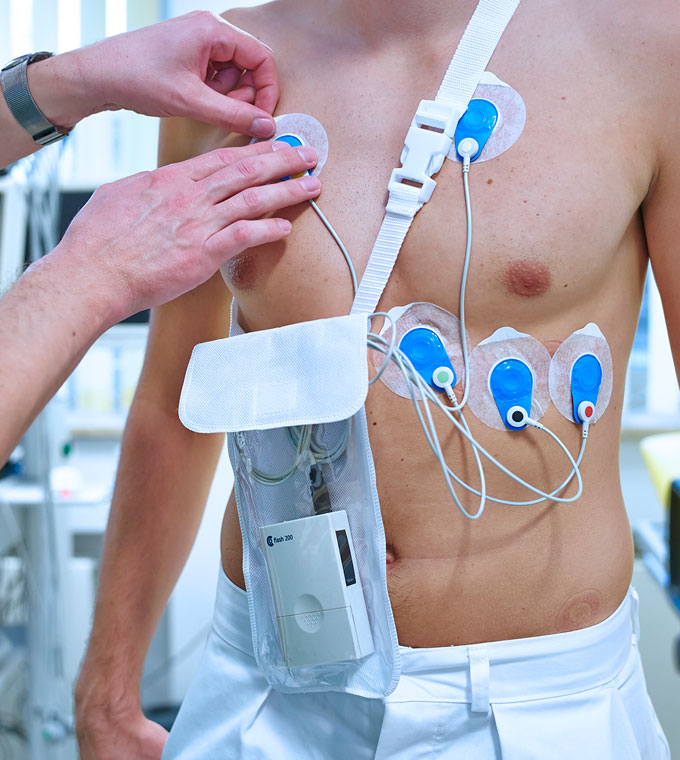
Long-term ECG including 7-day Holter monitor, telemetry
The patient usually wears a portable ECG device for 24 hours, sometimes up to a week, to record the long-term ECG. It is primarily used for rhythm diagnostics.
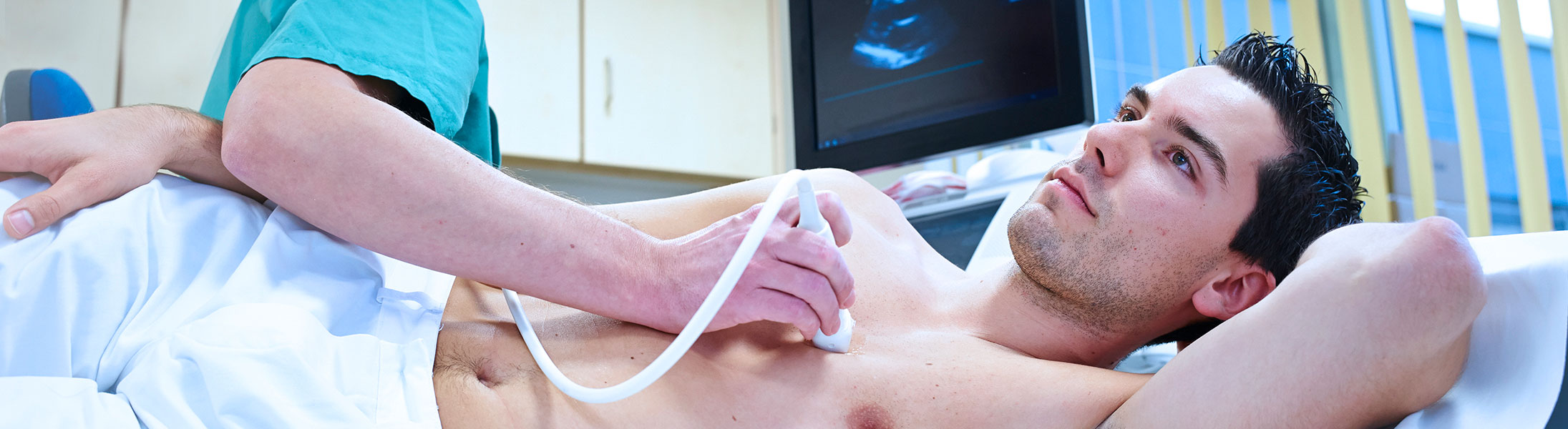
echocardiography
By placing a special ultrasound probe on the skin, all structures of the heart are displayed in real time using a black-and-white cross-sectional image.
In particular, the size of the heart chambers, valve function and the pumping function of the heart are clearly visible, allowing the ejection fraction of the heart to be determined. By using various Doppler techniques (colour Doppler, PW and CW Doppler), the function of the heart valves can be assessed, in particular the visualisation of insufficiencies (leaks) and stenoses (narrowings).
By placing a special ultrasound probe on the skin, all structures of the heart are displayed in real time using a black-and-white cross-sectional image.
In particular, the size of the heart chambers, valve function and the pumping function of the heart are clearly visible, allowing the ejection fraction of the heart to be determined. By using various Doppler techniques (colour Doppler, PW and CW Doppler), the function of the heart valves can be assessed, in particular the detection of insufficiencies (leaks) and stenoses (narrowing).
Here, a probe (similar to an endoscope used in a gastroscopy) with an ultrasound transducer at its tip is swallowed to assess the heart and aorta through the stomach wall and oesophagus.
This allows structures in the left atrium (blood clots, heart valve defects) to be assessed more accurately, as sources of interference such as rib bones and air in the lungs are eliminated. Patients who cannot be adequately examined using transthoracic echocardiography also benefit from this minimally invasive method.
Three-dimensional echocardiography can be performed both transthoracically (from the outside), for example to assess the heart valves, heart size, mass and function, and transoesophageally (through the oesophagus).
In addition to assessing heart valves, congenital heart defects and heart tumours, this method also creates optimal conditions for surgical or interventional procedures that can be accompanied by this method (heart valve closure, closure of an atrial septal defect). The 3-dimensional images provide the examiner with realistic views of the structures being examined.
Stress echocardiography is an echocardiography performed under stress.
The most common indication for a stress echo is suspected circulatory disorders in coronary heart disease. Here, after recording the heart function at rest, a defined stress test is performed either on a bicycle ergometer or using stress medication. Under stress, the heart function is now assessed regularly, paying attention to movement disorders of the individual heart muscle segments, which may indicate circulatory disorders.

Ultrasound/Doppler examination
Examination of the carotid arteries using ultrasound and PW Doppler provides indications of narrowing of the vessels (arteries) due to so-called plaques, which can increase the risk of stroke.
This enables patients to receive advice and targeted treatment regarding risk factors for stroke and heart attack. Patients with critical narrowings can be identified in good time and referred for definitive treatment (surgery, stent implantation).
Examination of the carotid arteries using ultrasound and PW Doppler provides evidence of narrowing of the vessels (arteries) due to so-called plaques, which can increase the risk of stroke.
This enables patients to receive advice and targeted treatment regarding risk factors for stroke and heart attack. Patients with critical narrowings can be identified in good time and referred for definitive treatment (surgery, stent implantation).
If peripheral arterial disease (PAD) is suspected, ultrasound examination is the first method of choice.
Calcium deposits and narrowing can be visualised. If walking distance is significantly restricted and narrowed or blocked arteries are suspected, the pelvic and leg arteries should be examined more closely, for example using CT or MRI angiography.
The doctor can often get an initial indication of the presence of a circulatory disorder from the patient's description of their symptoms. A typical symptom is pain in the leg (buttocks, thigh, lower leg and/or foot) after walking a certain distance, which improves when standing still – known as ‘intermittent claudication’. Further indications can be obtained from a physical examination of the patient, in particular by feeling the pulses in the feet on both sides – normally, the pulse can be felt strongly up to the back of the foot.
Swelling in the legs – usually more pronounced on one side – can be a sign of thrombosis (blockage of blood flow) in the deep veins of the legs.
Duplex sonography of the pelvic and leg veins is therefore mostly used to detect or rule out thrombosis in the pelvis, thigh or lower leg area.
To rule out thrombosis, the breath-modulated flow in the deep pelvic veins is first tested in the groin area (known as the Valsalva manoeuvre). Below the inguinal ligament, compression sonography is the method of choice; the veins must be clearly compressible in each section of the vessel. Duplex sonography also provides valuable additional information on the flow behaviour of venous blood; for example, problems with the venous valves can be visualised and assessed.
Occlusion pressure measurement is a non-invasive, risk-free and non-stressful method used to check the blood flow in both legs.
The examination is performed while lying down and takes approximately 10 minutes. The patient must lie down for 10 minutes before the examination begins. A blood pressure cuff is used to measure the (systolic) blood pressure on both upper arms and both lower legs. A Doppler probe is used to determine when the vessel opens or when the blood flows. The blood pressure values measured on the upper arm and lower leg are used to calculate the ankle-brachial index. The index is used to diagnose peripheral arterial occlusive disease (‘intermittent claudication’), to assess haemodynamic compensation, to monitor progress and to estimate cardiovascular risk (probability of cardiovascular disease such as stroke or heart attack).
This is an ultrasound examination of the thyroid gland – a simple, quick and non-invasive method that provides reliable results.
The examination is performed while lying down and takes approximately 5 to 10 minutes. This examination can be used to determine structural changes and thyroid size. Typical diseases for which this method is used are: hyperthyroidism and hypothyroidism, thyroiditis, goitre (struma) and thyroid cancer.
Further examination options
Bei diesem Thema fehlt ein Einstiegstext, consectetuer adipiscing elit. Aenean commodo ligula eget dolor. Aenean massa.
Donec pede justo, fringilla vel, aliquet nec, vulputate eget, arcu. In enim justo, rhoncus ut, imperdiet a, venenatis vitae, justo. Phasellus viverra nulla ut metus varius laoreet. Quisque rutrum. Aenean imperdiet. Etiam ultricies nisi vel augue. Curabitur ullamcorper ultricies nisi. Nam eget dui. Etiam rhoncus. Maecenas tempus, tellus eget condimentum rhoncus, sem quam semper libero.
During the tilt table test, the patient lying on a tilt table is passively raised by 60-80° after 15 minutes of lying down and kept in this position for up to 45 minutes.
This examination is used to clarify unexplained loss of consciousness, for example in cases where blood pressure does not adjust to rapid changes in position or reflex-mediated loss of consciousness (e.g. fainting after standing upright for a long period of time).
Long-term blood pressure monitoring is a simple and risk-free method of creating a blood pressure profile over 24 hours.
Blood pressure readings are measured automatically using a portable device, every 15 minutes during the day and every 30 minutes at night.
This method serves to:
- Confirmation or exclusion of a diagnosis of high blood pressure.
- Monitoring of treatment.
- Recording of critical episodes of high blood pressure, such as those that occur in certain diseases or in cases of difficult-to-control high blood pressure.
- Creation of a day-night rhythm profile. In certain diseases, this blood pressure rhythm is disturbed, and in some cases, causal treatment is possible.
The carotid pressure test is a simple clinical function test used to diagnose carotid sinus syndrome.
The test is performed with ECG monitoring and continuous blood pressure measurement. The examiner massages the baroreceptors of the carotid sinus in the area of the carotid artery bifurcation for approximately 10 seconds (after ruling out severe calcification). If the massage causes asystole lasting more than 3 seconds or a drop in systolic blood pressure of more than 50 mm Hg, hyperactive carotid sinus is likely to be present, which can lead to loss of consciousness.
certificates




Contact Cardiology and Internal Intensive Care Medicine

Dr. med. Andreas Brugger (englischer Eintrag)
Specialist in internal medicine/cardiology
Additional qualifications:
Interventional cardiology (DGK)
Specialised rhythmology (DGK)
Intensive care
Emergency/rescue medicine

Contact
Albert-Schweitzer-Straße 10
95326 Kulmbach
Cornelia Krauß
Phone 09221 98-1851
Fax 09221 98-1802
E-mail cornelia.krauss@klinikum-kulmbach.de


