This ward treats patients with acute life-threatening conditions across the entire spectrum of internal medicine. This includes patients with diseases of the heart and blood vessels, lungs, internal organs in the abdominal cavity, brain and the rest of the nervous system.
The symptoms include:
- acute coronary syndrome (heart attack) to cardiogenic shock (circulatory collapse due to
- heart failure)
- cardiac arrhythmias (e.g. ventricular fibrillation)
- pulmonary oedema (fluid leakage from the blood vessels into the lung tissue)
- pulmonary embolism (blockage of a pulmonary artery by a blood clot)
- severe pneumonia (lung inflammation) to ARDS (acute respiratory distress syndrome = acute lung failure)
- status asthmaticus (prolonged asthma attack)
- exacerbated COPD (acute worsening of chronic obstructive pulmonary disease)
- gastrointestinal bleeding (bleeding in the gastrointestinal tract)
- severe acute pancreatitis (inflammation of the pancreas)
- sepsis (blood poisoning)
- kidney failure
- status epilepticus (prolonged seizure)
- severe strokes
- and other clinical pictures
range of services
In addition to monitoring the patient's circulatory and respiratory functions, the comprehensive technical equipment includes advanced haemodynamic monitoring using the PiCCO system, modern ventilators with the option of invasive and non-invasive ventilation, and various renal replacement therapies.
Therapeutic cooling after cardiac arrest has long been routinely performed. In cases of severe heart or lung failure, extracorporeal membrane oxygenation (ECMO) is available as an organ replacement procedure.
The following is a brief overview of the diagnostic and therapeutic procedures used:
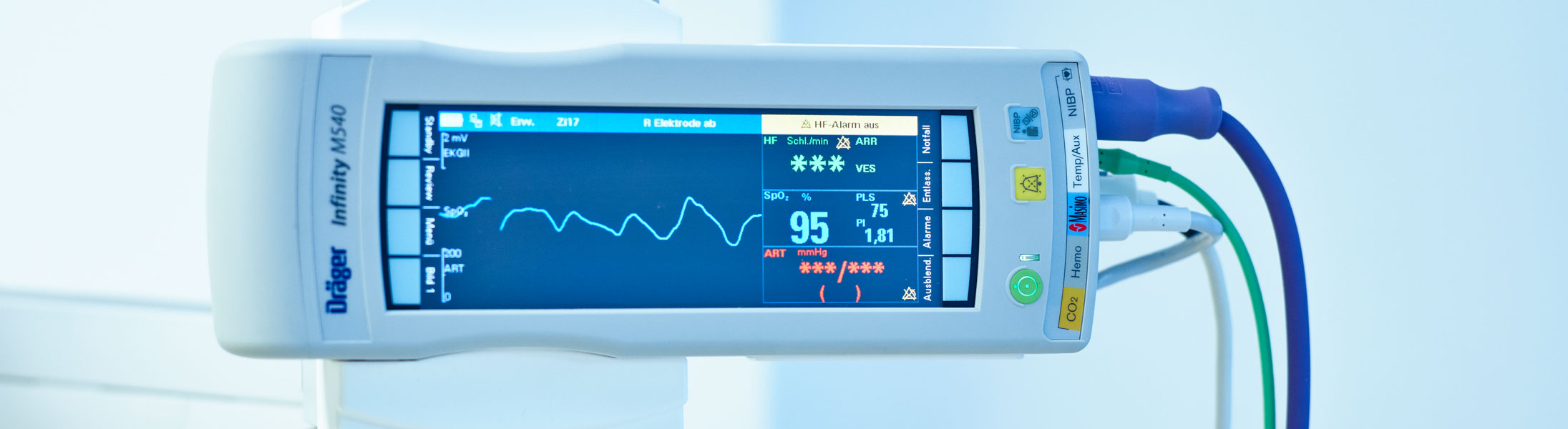
This refers to a combination of devices used to monitor the patient's circulatory parameters.
Circulatory parameters include heart rate, which is recorded by an electrocardiogram (ECG). It also includes blood pressure, which is measured either non-invasively using an upper arm cuff or invasively via cannulation of the arm or femoral artery, as well as oxygen saturation and body temperature. If there are any deviations from normal values, acoustic alarms are triggered in the ward. These are collated in the base centre, enabling the team caring for the patient to respond promptly.
PiCCO, bedside echocardiography and sonography are available for advanced haemodynamic monitoring. PiCCO is a device developed by a specialist company which uses two measurement methods (thermodilution and pulse contour analysis) to optimally control the patient's treatment (fluid administration and circulatory support medication).
The ventilator (respirator) can either assist or completely take over the patient's breathing. This can be done as non-invasive ventilation via a mask, for example in the event of a deterioration in a pre-existing chronic lung disease or acute pulmonary oedema. If a tube (ventilation tube) is inserted into the windpipe through the mouth or nose, this is referred to as invasive ventilation.
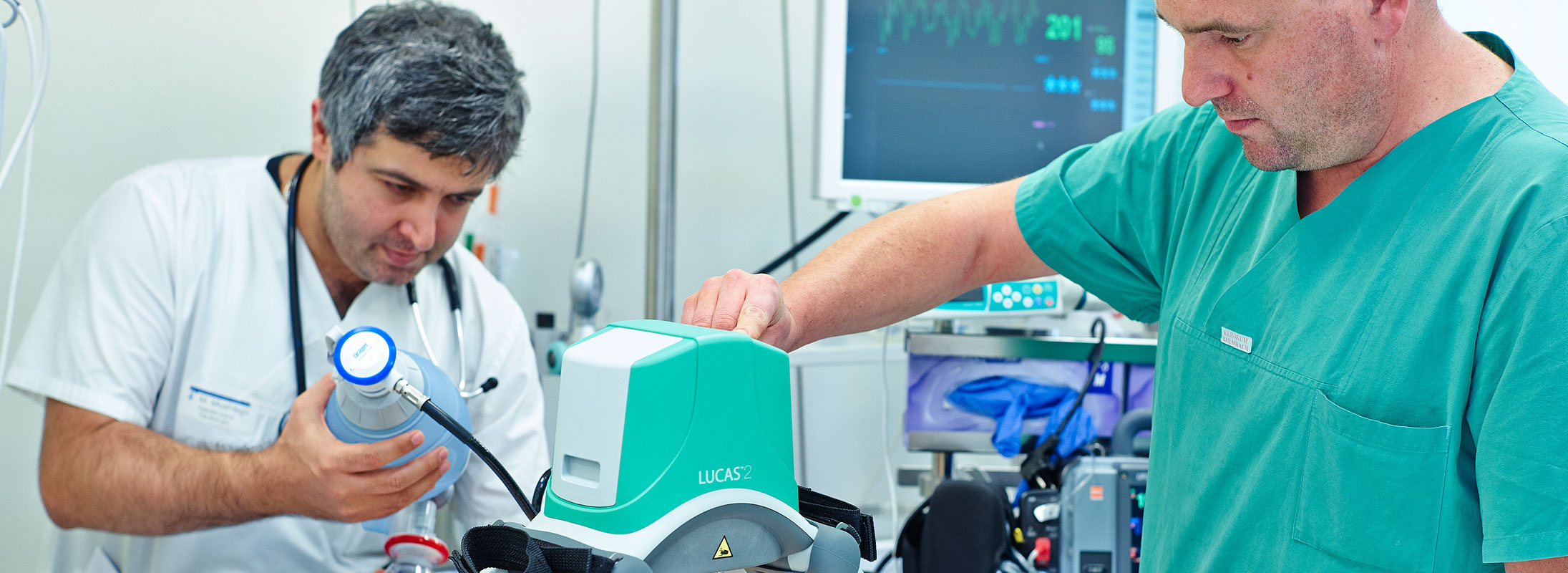
In the event of cardiac arrest, a mechanical resuscitation aid is available which automatically performs chest compressions once it has been applied. This allows the intensive care team to concentrate on treating the patient.
Patients who are successfully resuscitated after cardiac arrest, for example ventricular fibrillation during an acute heart attack, benefit from therapeutic cooling in terms of their neurological outcome (probability of long-term neurological damage). This is carried out using a special cooling catheter, which is inserted into the femoral vein. This method allows cooling and, in particular, rewarming to be controlled very effectively.
These are implanted in the cardiac catheterisation laboratory, with further treatment taking place in our intensive care unit.
The term dialysis refers to a blood purification procedure used to replace kidney function in cases of renal failure. The dialysis procedures available on the ward are either intermittent haemodialysis in cooperation with the nephrology department or continuous veno-venous haemofiltration (CVVH).
The bronchoscopy (examination of the airways) with the option of mucus suction is performed at the bedside in cooperation with the pulmonology department.
If artificial ventilation is expected to be required for a longer period of time, e.g. in cases of ARDS (Acute Respiratory Distress Syndrome = acute lung failure) or if weaning from the ventilator proves difficult, a tracheotomy (incision in the windpipe) may be necessary. In percutaneous dilatation tracheotomy, the windpipe is punctured from the outside using a hollow needle and a guide wire is inserted. A bronchoscopy is used to check the correct position of the wire in the windpipe, and then the access is widened using a plastic dilator via the wire until a breathing tube can be inserted. This procedure is performed by our pulmonology department.
certificates




Contact Cardiology and Internal Intensive Care Medicine

Dr. med. Andreas Brugger (englischer Eintrag)
Specialist in internal medicine/cardiology
Additional qualifications:
Interventional cardiology (DGK)
Specialised rhythmology (DGK)
Intensive care
Emergency/rescue medicine
Internal intensive care medicine
Ralf Dorfschäfer
Healthcare and nursing staff
Specialist nurse for anaesthesia and intensive care medicine AHA - ACLS provider
Contact
Albert-Schweitzer-Straße 10
95326 Kulmbach
Phone 09221 98-4790
Visiting hours and appointments
Daily from 2:30 p.m. to 6:00 p.m.
Individual arrangements with the responsible nurse are possible at any time.
In the interests of your relative and other patients, we ask you to make arrangements within the family so that, as a rule, no more than two relatives visit at the same time.