The functional department has two state-of-the-art catheter measurement stations. These are a bi-plane and a mono-plane system.
The laboratories are on call 24 hours a day for the immediate treatment of patients with acute heart attacks. One of their main tasks is the invasive detection of significant coronary heart disease (cardiac catheterisation).
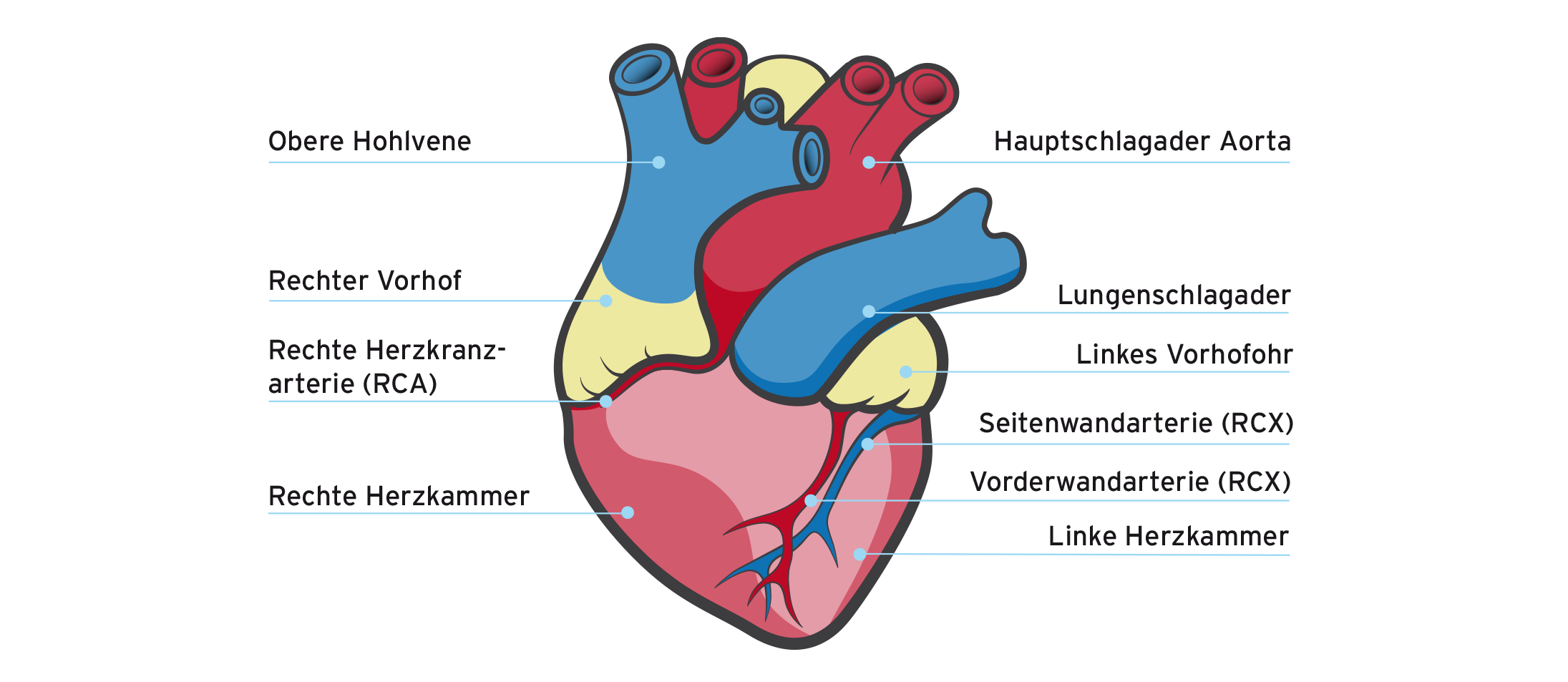
The heart, anatomy and structure
Treatment focus areas Interventional cardiology
Cardiovascular diseases are among the most common in the United Kingdom.
If suitable higher-grade narrowings are detected, the vessel is usually dilated using a balloon catheter and a stent (vascular support) is then implanted.
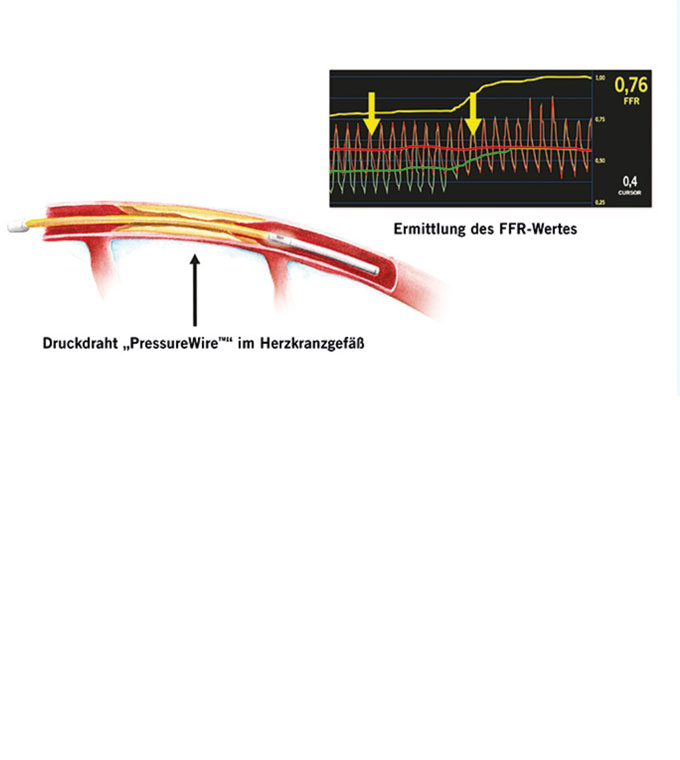
The most suitable method for assessing the relevance of a narrowing in the coronary vessels is the so-called pressure wire measurement.
Once maximum coronary blood flow has been reached, the relevance of the degree of stenosis can be estimated based on the pressure drop in the area of the narrowing. The further therapeutic procedure (conservative versus implantation of a vascular stent) then depends on the result of this examination.
Pressure measurement before (red curve, pa) and after (yellow curve, pd) a vascular narrowing. The relevance of a lesion can be determined from the pa/pd quotient under maximum blood flow. Courtesy of St. Jude Medical.
This method allows the plaque structure and the lesion to be visualised directly.
In addition, this procedure can be used to assess the quality of the intervention performed.
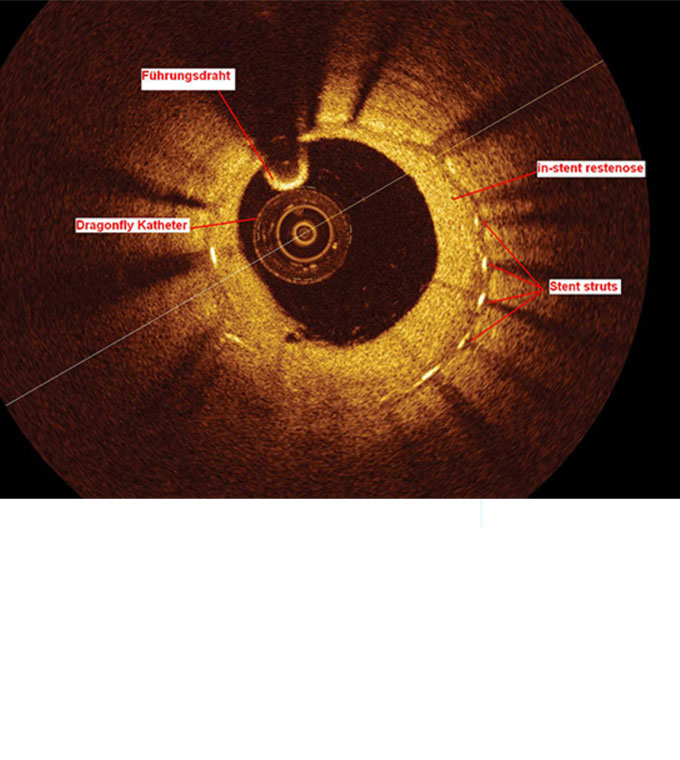
This is a modern, high-resolution procedure that is particularly useful for determining the diameter of a vessel with great precision. It can also be used to determine the length of a lesion (length of the narrowing of the vessel) in the case of a constriction. The procedure is mainly used to visualise modern vascular supports made of lactic acid.
OCT image of the cross-section of a coronary vessel after implantation of a modern vascular support (stent) with very thin struts. The OCT catheter can be seen in the centre. Courtesy of St. Jude Medical.
This procedure is used for severely calcified coronary arteries that cannot be dilated using conventional methods.
A miniaturised drill head can be used to easily overcome severely calcified narrowing of the artery. The artery can then be further dilated using balloons and finally fitted with a stent (vascular support).

This involves a balloon pump and a miniaturised heart-lung machine. These systems are used to support circulation in patients with severe heart failure.
In this form of treatment, two electrodes are implanted in the area of the ventricular septum of the right ventricle and in the area of the right atrium. These are connected to a pacemaker-like device (optimizer), which is usually placed below the right or left collarbone. The implantation technique is almost identical to that used for a conventional pacemaker implantation. The device stimulates the heart muscle during the absolute refractory phase. This does not lead to ventricular contraction, but rather to a complex influence on the calcium metabolism of the heart muscle cells. Ultimately, this results in an increase in cardiac output. For patients with severe heart failure, this primarily improves their quality of life and resilience.
In recent years, stent implantation in this vascular region has become established as an alternative to surgery on the neck vessels.
This procedure allows us to offer a high level of safety in our treatment focus.
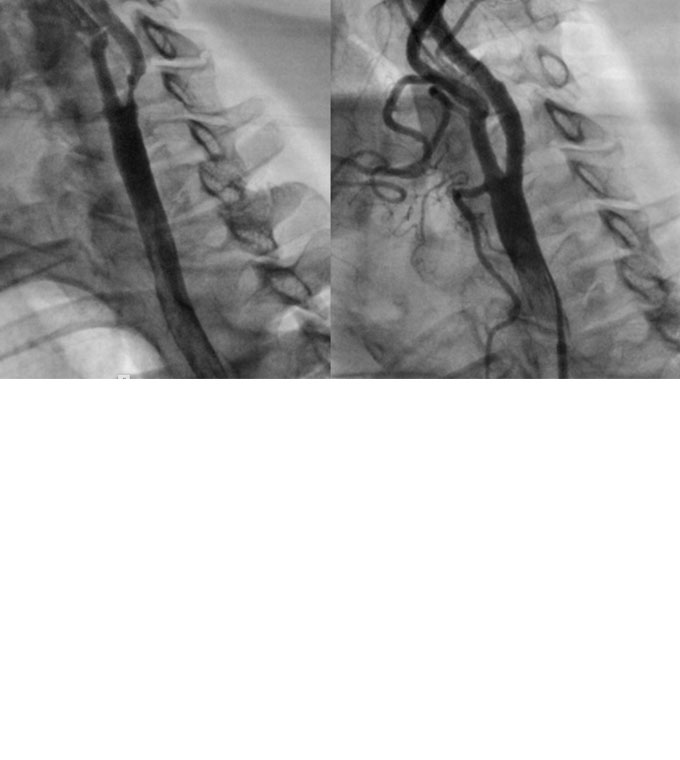
Left: Severe narrowing of the carotid artery before the intervention. Right: Result on the carotid artery after implantation of a vascular stent (CAS). The narrowing has been completely eliminated.
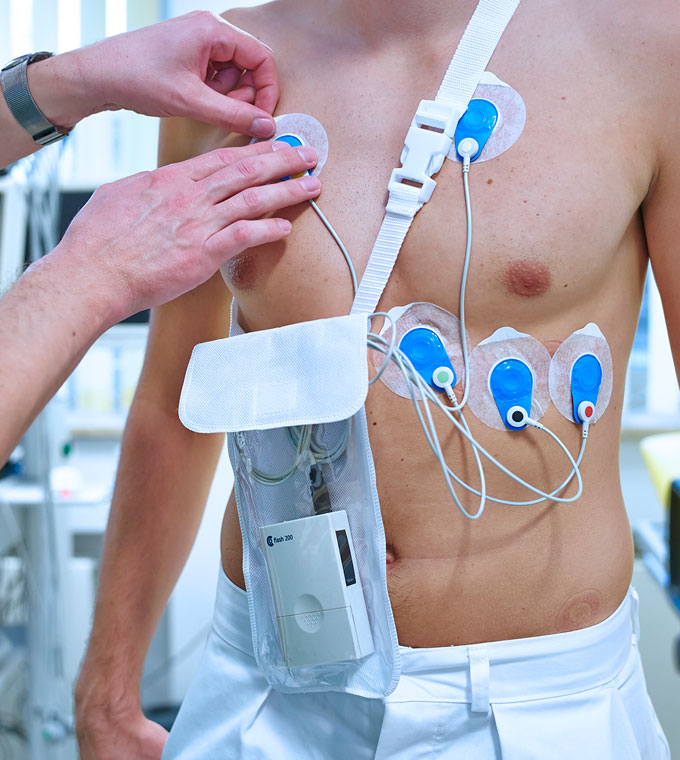
[Translate to English:] Das kleine in einer Umhängetasche oder am Gürtel tragbare Aufzeichnungsgerät nimmt EKG-Signale, wahlweise mit 3 oder 12 Ableitungen, über 24 bis 72 Stunden auf.
Dieses interventionelle Verfahren kann bei hochgradigen Engstellen der Nierenarterien in Sonderfällen zum Einsatz gebracht werden.

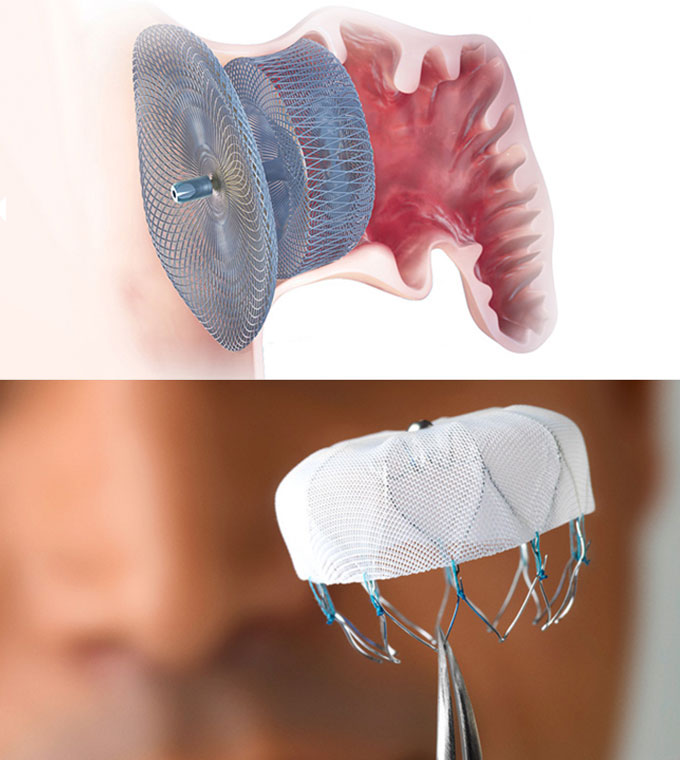
Common defects of the atrial septum are the persistent foramen ovale (PFO) and atrial septal defect (ASD).
Both can be treated with interventional procedures if indicated. This involves inserting a so-called occluder (small umbrella) into the area of the defect to seal it.
Link to the film?
A myocardial biopsy (removal of heart muscle tissue) is performed on patients suspected of having heart muscle disease or cardiac storage disease as the cause of heart failure or cardiac arrhythmia.
Under X-ray guidance, heart muscle tissue is removed from the right and/or left ventricle using tiny forceps.
The left atrial appendage is a pouch in the left atrium of the heart. Blood clots often form in this pouch in patients with atrial fibrillation. These clots act as a source of embolism and trigger strokes. Atrial fibrillation is the most common cardiac arrhythmia in the United Kingdom.
Patients with atrial fibrillation and certain risk factors usually have to undergo blood-thinning therapy. If serious side effects occur (cerebral haemorrhage, bleeding from the gastrointestinal tract), the atrial appendage can be closed interventionally with a special umbrella device. Blood thinning with Marcumar or another substance can then be discontinued. This is intended to prevent further bleeding complications for the patient. Depending on the anatomy of the left atrial appendage, different closure systems are used. Below are images of the most commonly used devices in Germany for closing the left atrial appendage.
Image: ACP umbrella for closure of the left atrial appendage, courtesy of St. Jude Medical.
Schematic representation of the position of an ACP umbrella in the LAA, courtesy of St. Jude Medical.
Umbrella (Watchman device) for closure of the left atrial appendage, courtesy of Boston Scientific.
Computed tomography (CT) and magnetic resonance imaging (MRI)
Cardiac MRI and cardiac CT examinations are offered in collaboration with the radiology department at Kulmbach Hospital. Common indications for these imaging procedures include suspected coronary heart disease following an inconclusive or unfeasible stress test, suspected coronary artery abnormalities, or signs of heart muscle inflammation (myocarditis). Cardiac MRI can also help in the diagnosis of heart muscle diseases.
Interventional heart valve repair – a new procedure at Kulmbach Hospital
Heart failure is a condition in which the heart cannot pump enough blood around the body.
The heart tries to compensate for this by enlarging, and this enlargement causes the mitral valve (the valve between the left atrium and ventricle) to widen, which in turn leads to mitral valve leakage and mitral regurgitation. Unfortunately, this further impairs the function of the heart, causing heart failure to worsen over time.
Functional mitral regurgitation (FMR) is caused by the mitral valve not closing properly, allowing blood to flow in the wrong direction or backflow. This reduces the amount of oxygenated blood pumped to the body, increases the symptoms associated with heart failure and reduces the quality of life of those diagnosed. Approximately 70 per cent of people with heart failure suffer from FMI.
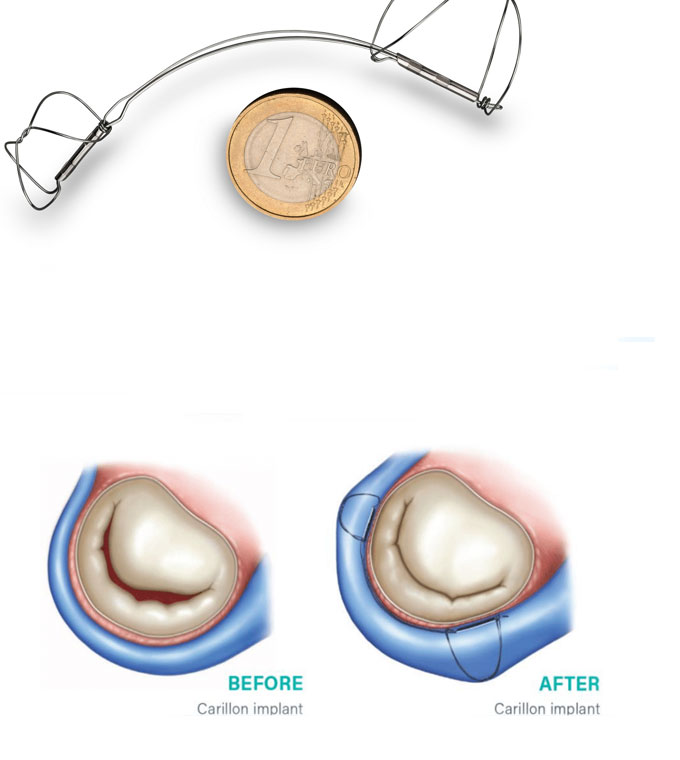
The Carillon Mitral Contour System is a minimally invasive treatment option specifically designed to treat FMI. The Carillon implant is placed in a vein on the outside of the heart adjacent to the mitral valve using a non-surgical, minimally invasive (catheter-based) technique. This simple procedure is designed to reshape the mitral valve, reduce valve leakage and thus reduce mitral regurgitation.
Results from several international clinical studies show that the Carillon system effectively reduces mitral regurgitation. Patients treated with the Carillon system generally experience an improvement in heart failure and overall quality of life.
We are delighted that we have been able to offer our patients this minimally invasive method of treating mitral valve leakage for several months now.
Yours sincerely, Dr J. Trautvetter
range of services
cardiac catheterisation
- RHK
- Rest and stress
- PTCA
- PCI
- Implantation of coronary stents
- Drug-coated balloon catheters (DCB)
- Drug-eluting balloon catheters (DEB)
Procedure for assessing the coronary arteries
For the assessment and visualisation of deposits and damage to the inner walls of blood vessels
High-resolution method for determining vessel diameter, lesion length and visualisation of vascular supports
Procedure for diagnosing recurrent chest pain
Method for overcoming severely calcified vessels with the aid of a miniaturised drill head
- Intra-aortic balloon pump (IABP)
- Cardiohelp (miniaturised heart-lung machine)
- ECMO (extracorporeal membrane oxygenation), intensive care technology for maintaining respiratory function
X-ray imaging of the carotid artery using contrast medium (DSA = digital subtraction angiography)
CAS, Implantation von Gefäßstützen als Alternative zur Operation
In cases of narrowing of the renal arteries
- Atrial septal defect (ASD) (hole in the heart wall)
- Persistent foramen ovale (PFO) for stroke prevention
Tissue sampling from the heart muscle in cases of suspected heart muscle disease or existing heart muscle weakness, as well as cardiac arrhythmia
For the prevention of embolism and stroke in patients with atrial fibrillation
For the prevention of embolism and stroke in patients with atrial fibrillation
Interventional heart valve repair – a new procedure at Kulmbach Hospital
Heart failure is a condition in which the heart cannot pump enough blood around the body.
The heart tries to compensate for this by enlarging, and this enlargement causes the mitral valve (the valve between the left atrium and ventricle) to widen, which in turn leads to mitral valve leakage and mitral regurgitation. Unfortunately, this further impairs the function of the heart, causing heart failure to worsen over time.
Functional mitral regurgitation (FMR) is caused by the mitral valve not closing properly, allowing blood to flow in the wrong direction or backflow. This reduces the amount of oxygenated blood pumped to the body, increases the symptoms associated with heart failure and reduces the quality of life of those diagnosed. Approximately 70 per cent of people with heart failure suffer from FMI.
The Carillon Mitral Contour System is a minimally invasive treatment option specifically designed to treat FMI. The Carillon implant is placed in a vein on the outside of the heart adjacent to the mitral valve using a non-surgical, minimally invasive (catheter-based) technique. This simple procedure is designed to reshape the mitral valve, reduce valve leakage and thus reduce mitral regurgitation.
Results from several international clinical studies show that the Carillon system effectively reduces mitral regurgitation. Patients treated with the Carillon system generally experience an improvement in heart failure and overall quality of life.
We are delighted that we have been able to offer our patients this minimally invasive method of treating mitral valve leakage for several months now.
Yours sincerely, Dr J. Trautvetter

Frequently asked questions
The catheter examination can take varying amounts of time, depending on the complexity of your examination. We usually need 10 minutes for preparation, 10 minutes for the examination itself and another 5 minutes for follow-up. You can then return to your ward.
The examination is performed under local anaesthetic. Access is gained via the groin or wrist. You will feel a sensation of pressure. You will not feel any pain inside the blood vessels or in the heart chamber itself, as there are no pain receptors there.
The catheter examination can take varying amounts of time, depending on the complexity of your examination. We usually need 10 minutes for preparation, 10 minutes for the examination itself and another 5 minutes for follow-up. You can then return to your ward.
[Translate to English:] Da nur eine örtliche Betäubung erforderlich ist, bleiben Sie wach und ansprechbar. Ein Gespräch mit dem untersuchenden Arzt ist jederzeit möglich. Beruhigungsmittel benötigen Sie in der Regel nicht. Gegebenenfalls können Sie diese nach Wunsch und in Absprache mit dem behandelnden Arzt jedoch erhalten.
[Translate to English:] Die Herzkatheteruntersuchung wird seit etwa 50 Jahren durchgeführt. Die Entwicklung der Untersuchungstechnik und der zur Verfügung stehenden Materialien haben es in diesen Jahren ermöglicht, dass es sich trotz der Komplexität um eine risikoarme, zuverlässige Routineuntersuchung für Diagnose und Behandlung der Herzerkrankungen handelt. Es ist immer noch die zuverlässigste Methode, um den Zustand der Herzkranzgefäße darzustellen.
Die häufigste Untersuchung ist der Linksherzkatheter. Er beschäftigt sich mit der linken Seite des Herzens (dem arteriellen Bereich) und kann sowohl die Herzkammer als auch die Kranzgefäße und die Hauptschlagader (Aorta) darstellen. Durch diese Messungen lassen sich die Eigenschaften des Blutkreislaufs, die Pumpleistung des Herzens und die Herzklappenfunktionen beurteilen.
Durch einen Rechtsherzkatheter erhält man Informationen über die rechte Seite des Herzens (den venösen Bereich), die Druckverhältnisse in der rechten Herzkammer, die Lungengefäße und indirekt auch den Druck im linken Vorhof.
Sieht der Untersucher Verengungen an den Herzgefäßen, können diese in gleicher Sitzung aufgedehnt und mit einem Stent (Gefäßstütze) versorgt werden.
Handelt es sich um eine fortgeschrittene Erkrankung der Koronarien (Herzkranzgefäße), bespricht der Untersucher den Befund mit Ihnen nach Beendigung der Untersuchung. In diesem Gespräch werden Ihnen Vorschläge zur Weiterbehandlung aufgezeigt und das weitere Vorgehen besprochen.
Cardiac catheterisation is now a routine procedure. At our clinic, approximately 2,000 procedures are performed each year by experienced doctors. However, it is not without potential complications; these are mostly problems at the puncture site (bruising, haematoma). Serious complications (such as cardiac arrest, stroke, thrombosis) are very rare and usually affect critically ill patients or emergencies.
Occasionally, contrast agent intolerances (such as skin rash, feeling of heat or nausea) occur, which usually disappear after a few minutes. An information session on the day before the examination is mandatory and is conducted by the ward doctor. All possible complications are listed on the form; please discuss these in detail with your ward doctor. This list must be provided for legal reasons, even if these complications are very rare. During this consultation, please ensure that you inform the doctor of any pre-existing conditions you are aware of (e.g. known allergies, bleeding tendency or kidney dysfunction).
During a left heart catheterisation, the doctor punctures an artery, as this provides direct access to the heart (arterial area) via the aorta. During a right heart catheterisation, a vein is punctured in order to access the right side of the heart (venous area) via the vena cava.
After administering a local anaesthetic, the vessel is punctured using a puncture needle. A very soft guide wire is inserted into the vessel through this needle.
After the needle is withdrawn, a sheath (a small plastic tube with a diameter of 1.4–1.8 mm and a valve to prevent blood leakage) is inserted into the blood vessel over the wire.
Through this sheath, the differently shaped catheters can now be advanced to the heart one after the other under X-ray control. However, the patient does not feel anything, as the vessels have no pain receptors.
These catheters (which are shaped hollow tubes) can be used to inject contrast medium to visualise the coronary vessels, measure pressure and take blood samples to measure oxygen levels.
After these visualisations and measurements, your examiner can make a diagnosis.
- Are there any narrowings in the coronary arteries?
- How many and where are they located?
- Are they significant and therefore require treatment?
- Are any coronary arteries completely blocked?
In uncomplicated cases, vasodilation can be performed immediately afterwards. If there are more complex changes that may require surgery, the examination is concluded at this point. The sheath is removed.
If the examination was performed via the groin, an elastic bandage is applied around the hips to create a pressure bandage. For examinations performed via the wrist, a cuff is placed around the wrist (similar to a watch strap) and the puncture site is compressed using an air cushion.
Bei unkomplizierten Fällen ohne Eingriffsmaßnahmen kann der Patient am selben Tag entlassen werden. Bei Problemen an der Punktionsstelle sollte der Patient über Nacht in der Klinik bleiben. Bei Gefäßaufdehnungen, mit oder ohne Implantation einer Gefäßstütze, (Stent) empfiehlt sich ein Aufenthalt von ein bis zwei Tagen. Das richtet sich jeweils nach dem Schweregrad Ihrer Erkrankung.
As the puncture site is very small, it heals quickly. The patient can usually get up immediately or after 4 hours. However, strenuous physical activity should be avoided for the first 3 to 4 days.
Thanks to many years of experience, increasingly delicate materials and the wealth of information obtained through this procedure, cardiac catheterisation has become a routine examination.
Nevertheless, the examination is only recommended in cases where heart disease is suspected.
The indication is based on the latest guidelines from the International and German Societies of Cardiology.
If you are taking Macumar, you should stop taking it beforehand. Please discuss this with your GP. The target INR value should be below 2.0.
It is essential that you continue to take 100 mg of ASA and 75 mg of clopidogrel. Please stop taking metformin for 3 days. You should continue to take your blood pressure medication and other medications.
certificates




Contact Cardiology and Internal Intensive Care Medicine

Dr. med. Andreas Brugger (englischer Eintrag)
Specialist in internal medicine/cardiology
Additional qualifications:
Interventional cardiology (DGK)
Specialised rhythmology (DGK)
Intensive care
Emergency/rescue medicine
Contact
Albert-Schweitzer-Straße 10
95326 Kulmbach
Cornelia Krauß
Phone 09221 98-1851
Fax 09221 98-1802
E-mail cornelia.krauss@klinikum-kulmbach.de
Office hours and appointments
Please call us to arrange an appointment.





